The CMS 1500 Form and Envelope
SpeedySoft USA provides a one-stop shop for all your medical stationary needs. Please select from our official claim forms and claim form envelopes below.
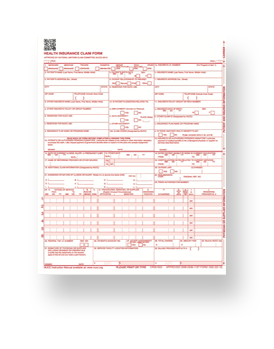
New CMS 1500 Claims Forms
The most up-to-date 02/12 version of the CMS 1500 claim form that is ICD 10 ready. Single sheet claim forms suitable for either ink jet or laser printers. Forms are completely compliant with the Medicare specifications.
Price Starts at $49.95

Envelopes for CMS 1500 Claim Forms
Please select from our two types of envelopes for use specifically with CMS 1500 insurance claim forms. Both feature Self Seal envelopes with no need for licking.